Half a year after receiving an official diagnosis of cognitive dysfunction from my neurologist and being recommended for various sorts of therapies, I’m finally off (one of) the waiting list(s) and in a “cognitive strategies group” for people with acquired brain injuries (ABIs).
I wasn’t sure what to expect. Originally, I thought cognitive remediation therapy might involve machines that go ‘ping’ and look like space pods; I’d sit inside on a gamer-type chair, all wired up, and use my mind to manipulate dots on the screen or solve problems with my eye movements. (Similar to how they brainwash people in movies, but in a good way.) Little by little, I’d build back neural pathways and forge new ones, emerging triumphantly after a few months of these sessions to cheers and hearty handshakes from the white-coated therapists who’d been monitoring my progress like NASA scientists. “You’ve done it!” they’d cry. “No one’s ever recovered so efficiently and so well! We’re sorry to see you go - it’s been an honor to watch your brain in action.”
(Writing this, I realize that I was basically picturing a CRT version of ‘Ender’s Game’. Such a good book; such a horrible author.)
Over time, however, I started to realize that cognitive rehabilitation was going to be a lot less high-tech (and a lot slower) than I had imagined. My first clue came when my neuropsych evaluations, both at leading neurological centers in super-fancy hospitals in NYC, involved nothing more modern than paper and a pencil. This was seconded by the fact that both therapists’s computers had the dingy yellow patina that cream-colored plastic casings acquire with time and use. The third clue was when I - still hoping in March to be back in the classroom in September - asked the second evaluator what I could do to make progress while waiting to get off the list for insurance-covered therapy (and while my amazing Dr. Altman, who isn’t covered by insurance, is on maternity leave), and the answer was “you could try writing down how long it takes you to do daily tasks, to get a performance baseline.”
I think this was the precise, crushing moment that I realized that I was in for the long haul. (The therapist then carefully recorded my mood as ‘anxious’ and ‘distressed’, which led to a call from my neurologist to see if I was ok.) No one was going to try to get me back in the classroom by September - I was “in the system” now, and I would be dealt with in the system’s time and at the system’s pleasure. Those white-coated brain scientists weren’t going to be shaking my hand any time soon.
When I asked again if there was anything I could do to help my brain while I waited to get off the lists for individual and group therapy, as opposed to just observing it, the doctor looked a bit confused and said, “I mean, you could learn something new - like, maybe take a class?”
I just sat there for a moment with my mouth a little open, staring at her. (This probably didn’t boost her confidence in my intellectual acumen.) A lifelong academic, all I could think was “I can’t take a class right now! How am I supposed to handle Econ or Physics or whatever?” And then I realized that she meant classes like ‘pottery lessons’ and ‘life drawing’, and I suddenly felt like a racehorse who’d stumbled at the Kentucky Derby and was being led into a big green pasture with a nice blue pond and told that this was her home now. No more racing, but look at the lovely trees - and there could be some dressage lessons!
Don’t get me wrong. Pottery classes and life drawing seminars are awesome and fun! (They are, in NYC, also intensely expensive.) I love doing craft-y things like knitting and embroidering and painting…although my ability to follow knitting patterns has taken a big hit and my fine-motor coordination isn’t always the best. It was more the thought that there I was, asking for anything to help me get back to where I’d come from and what I’ve always loved doing, and the best one of the top cognitive rehab centers in the country could offer was a recommendation for basket-weaving. (I looked basket-weaving up, out of curiosity. The courses in my area average $400 for 2-4 sessions. No promises are made about enhanced executive function, but the baskets do look pretty sweet.)
In any event, by the time I finally received the phone call telling me I could join a cognitive strategies group, my expectations were…not high. I’d gone from imagining space-age ‘we compete to help each other succeed’ game sessions to the group sessions from ‘One Flew Over the Cuckoo’s Nest’. “At least we meet on-line!” I thought to myself. “I will make myself a really excellent cup of coffee and get ready to take notes in my new Cog-Therapy-Specific notebook.” (Since apparently insurance considers this ‘mental health’ rather than ‘medical’ and thus doesn’t cover it, I was also thinking if it didn’t seem likely to be useful, I could gracefully bow out.)
The first meeting was, however, kind of amazing.
It was the first time I’ve been part of a conversation with other people who have an acquired brain injury, and the immediate sense of solidarity felt like climbing into a delightfully hot bath after a long, hard day - that tension-release shock of “Oh! I don’t have to try to explain: THEY KNOW!!” As we went around and introduced ourselves, explaining how we’d gotten there and what our main goals were, there was a lot of head-nodding and wry smiles from the other participants, and the signs of instant recognition were delightful.
It was actually fascinating how familiar the experiences the other participants described were - especially since there are maybe 8-10 people in the group, aged early 20’s to late 60’s, from all walks of life, and with a range of severity of disability and origin stories: several stroke survivors, a few people with white matter lesions, some accident/concussion survivors. (As usual, in this and any future discussion, I’ll avoid identifying details like names or - honestly, I don’t even know what else would count as identifying, since you don’t know which hospital or which group I’m part of! Anyway, not giving names will be easy because they’re lost in my working memory like tears in the rain in any event.)
In retrospect, I realized that although I’ve been surrounded by incredibly supportive friends and family this past year, I know almost no one who also has a life-changing ABI. I’m aware of a few people who have or had an ABI, mostly via Facebook or friends-of-friends, but the only person I’m close to who has one currently affecting their life also has aggressive stage 4 cancer, and so when we talk, the focus tends to be how their latest treatment is or isn’t affecting the tumors. This is all new to me, and it’s all new to almost everyone else I know as well. In my usual contexts and haunts, I ‘stick out’ a bit like an unsolved problem or an unknown quantity, and people aren’t quite sure what to expect when we get together, especially if they haven’t seen me in a while. On the one hand, this is totally fair, since I’m often not sure what to expect myself! On the other hand, some people have responded by either trying to ‘solve’ me with advice and assurances, or by avoiding the unknown (and, thus, me) altogether. I’m currently a big fan of the friends who take the awkward by the horns and just let us figure it out together.
In any event, I’m looking forward to future group meetings, not so much for the cognitive ‘strategies’ we’re supposed to be learning about via the group leaders, but for the simple together-ness of hearing someone else say, “I can never remember what that thing is called - my spouse always has to tell me.”
Ok, ok - I won’t pretend I’m all noble and will simply be soaking up the solidarity of my fellow ABI-ers. I’m also really looking forward to the extended people-watching! I’ve already got bets on with myself over who’s most likely to dominate group discussions, and who’s least likely to speak unless specifically prompted. Personally, I’m determined not to be ‘most likely to forget to show up’: I just set my alarms. It’s a bit like a new faculty orientation, where everyone watches each other while Campus Leaders share Helpful Information - except in this group we admit up front that we won’t remember each other’s names.
Next week I hope to have an update on the “NYC apartment: do we stay or do we go?” question. Until then, be nice to your noggins!




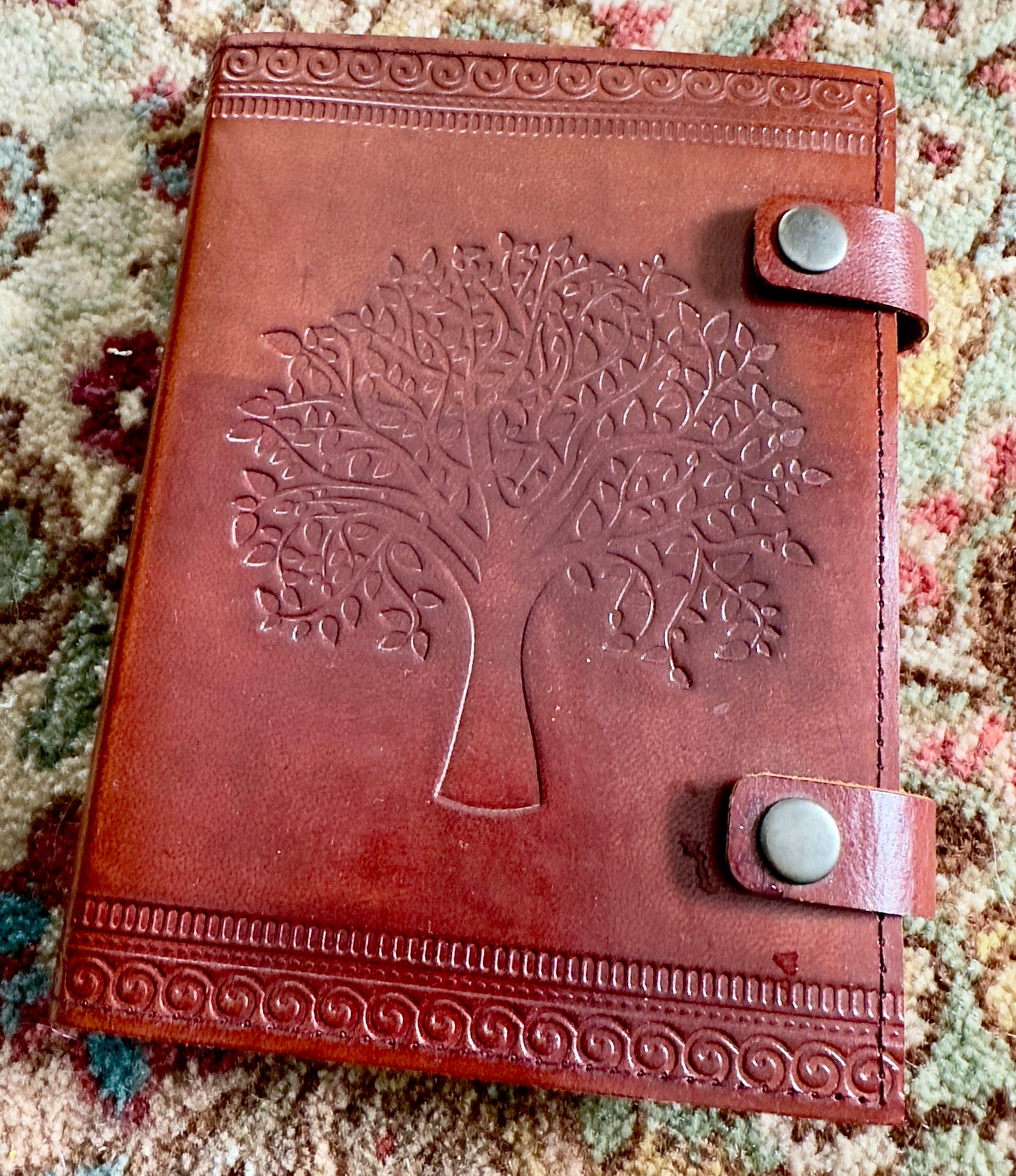

Yay, new stationery.
Loved this update